Platelets or thrombocyte cell fragments are characterized as small oval, spherical blood component with no nucleus, formed in the bone marrow and play a role in blood coagulation.
The normal quantity of platelets in the blood is about 150-450×109 / L of blood. The lifetime of platelets is 7-10 days. The blood component is degraded in the liver and spleen.
The spleen is a designated place of isolation in the body where the storage of blood cells is made, including platelets. Normally, the spleen sequesters approximately 1/3 of newly produced platelets.
It will be a really horrible situation to experience sudden and uncontrolled gushing out of blood from the nose, gums and other openings of the body. And sadly, it could happen with a really low platelet count. Before that happens, better manage it immediately (presented below is the risk of bleeding in patients with thrombocytopenia). This may usually be a costly endeavor but there are affordable options such as all-natural remedies you can learn from money back guaranteed materials like Conquer Low Platelets.
What causes low platelets? Decreased platelet count is called thrombocytopenia. According to gradiation, it can vary from moderate, moderately severe, and severe. With a lower cell count, the severity of the disease becomes bigger.
Low platelets causes a risk of bleeding in varied degrees in relation to the amount of drop which is mainly influenced by the causative factor involved. Let us take a look at each different potential degree of bleeding that can take place depending on the platelet level as detailed below:
| Platelet count | Risk of bleeding |
| >100.000/µL | No abnormal bleeding, even after surgery |
| 50.000–100.000/µL | The patient may bleed more than normal after serious injury |
| 20.000–50.000/µL | Hemorrhage comes at a smaller injury |
| <20.000/µL | The patient may bleed spontaneously |
Some of the Major Causes of Low Platelets or Thrombocytopenia:
1. Immune-mediated Thrombocytopenic Purpura
The immune-mediated thrombocytopenic purpura, also known as ITP is a condition marked by the development of antibodies against platelets. This attack of antibodies to normal cells is what causes low platelet count levels in patients with ITP. The condition may lead to a disorder described as immune-mediated thrombocytopenia.
Description of the two forms of ITP: acute and chronic.
The acute form is more common in children, and usually occurs after recovery from an infection. Frequently the patient has a non-specific viral infection. Although, there are times where acute ITP develops when recovering from a bacterial infection. While adults may also develop acute ITP, the disease occurs more often in gradual form (chronic ITP). Most adults do not remember whether it had been a viral or bacterial infection. Approximately 90% of ITP patients is younger than 40 years old. Interestingly, the chronic form of ITP affects women more frequently. Read ITP Treatment Methods.

2. Thrombocytopenia in pregnancy
Almost 5% of women develop thrombocytopenia during pregnancy. It is a cause of low platelets referred to as gestational thrombocytopenia, which should be distinguished not only from ITP, but also from other causes of thrombocytopenia associated with pregnancy, such as eclampsia, disseminated intravascular coagulation (DIC), HIV, Thrombotic thrombocytopenic purpura (TTP), and Hemolytic-uremic syndrome (HUS).
Clinical findings in favor of gestational thrombocytopenia, and against ITP will present a platelet count > 50,000 / uL and a history of thrombocytopenia during pregnancy. If the platelet count falls to <50,000 / uL, the patient should seriously consider the possibility of ITP. The diagnostic criteria for gestational thrombocytopenia are listed in the following table.
Diagnostic Criteria for Gestational Thrombocytopenia |
|
3. Infection
Infection is one of many low platelet count causes that has been commonly identified in patients. The main cause of thrombocytopenia by infection is viral in type. Among many other examples include infectious mononucleosis, CMV, and HIV. In most of the cases, the patient’s medical history may reveal recent symptoms consistent with viral infection.
Thrombocytopenia can be present in patients with HIV where it may be immune mediated or non-immunological in origin, but it seems that the majority of the cases have shown that the drop in platelet count has instead resulted from inefficient production of platelets.
It is not uncommon that the cause of the drop will depend on several factors. In addition to immune-mediated thrombocytopenia, thrombocytopenia in patients with HIV can happen due to suppression brought about by bone marrow granulomatous disease or probably induced by drugs. Moreover, the HIV immune mediated thrombocytopenia may occur at any time during HIV infection. It can even develop when the viral load is small, and the number of CD4 lymphocytes is relatively well preserved.
Thrombocytopenia, other than the connection with viral medical conditions, can also occur with infections that are caused by bacteria (gram-positive and negative) such as mycoplasma, rickettsia, as well as the parasitic infection malaria.

4. Malignant disease
Lymphoproliferative diseases such as chronic lymphatic leukemia and lymphoma may also be associated with immune-mediated thrombocytopenia, one of the common malignant disease-related low platelet causes.
However, more often the result of thrombocytopenia is due to a decrease in platelet infiltration of the bone marrow or probably because of cancer treatment with cytostatics.
Although immune-mediated thrombocytopenia is also described in patients with solid tumors, but the association is rare.
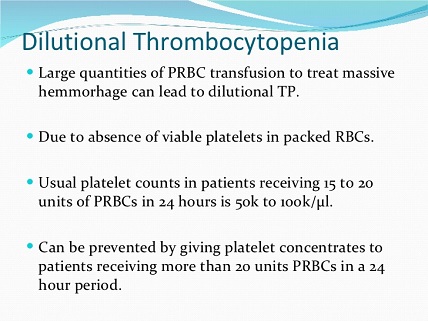
5. Dilutional thrombocytopenia
This is a common cause of thrombocytopenia in hospitalized patients who have lost a significant amount of blood. This happens when the aggressive application of intravenous transfusion is made and platelet count falls.
6. Radiation Specific
Radiotherapy can complicate the development of thrombocytopenia. It is one of the causes of low platelet count where damage occurs in the bone marrow affecting megakaryocytes causing the need to undergo certain processes before being able to circulate platelets. Thrombocytopenia typically occurs about 7-10 days after radiotherapy.
- Fang Chen, Mingqiang Shen, Dongfeng Zeng, Cheng Wang, Song Wang, Shilei Chen, Yong Tang, Mengjia Hu, Mo Chen, Yongping Su, Xinze Ran, Yang Xu, & Junping Wang (2017). Effect of radiation-induced endothelial cell injury on platelet regeneration by megakaryocytes.
- Sergo Mkhitaryan, Samvel Danielyan, Lilit Sargsyan, Lusine Hakobyan, Samvel Iskanyan, Samvel Bardakchyan, Ruzanna Papyan, Jemma Arakelyan, Karmen Sahakyan, Tatevik Avagyan, Armen Tananyan, Armen Muradyan, & Gevorg Tamamyan (2019). Younger age and previous exposure to radiation therapy are correlated with the severity of chemotherapy-induced thrombocytopenia.
- Williams M1, Liu ZW, Woolf D, Hargreaves S, Michalarea V, Menashy R, Kooner I, & Wilson E (2012). Change in platelet levels during radiotherapy with concurrent and adjuvant temozolomide for the treatment of glioblastoma: a novel prognostic factor for survival.
7. Drug-induced thrombocytopenia
Most of the medicament-related cases of thrombocytopenia is a result of any recently introduced drug during therapy. In fact, the time it takes for low platelet count to occur is only 2 weeks. Nevertheless, there have been described cases where the patient has already been taking medications for three years before a drop in platelet count displayed.
The diagnosis for drug-induced thrombocytopenia can be settled when the cease of use of the suspected drug resulted to having platelet count returning to normal levels. In most cases, thrombocytopenia draws 5-7 days after discontinuation of the drug. Sometimes thrombocytopenia lasts longer due to the slow elimination of the drug or its metabolites out of the body.
Although thrombocytopenia, after rechallenge can represent an even stronger diagnostic evidence, clinicians should always be in alert because re-provocation can be dangerous. Some patients react to display severe thrombocytopenia after a rechallenge with the drug. If the medicament is the culprit, re-provocation will lead to thrombocytopenia within three days of application.

- James N. George & Richard H. Aster (2017). Drug-induced thrombocytopenia: pathogenesis, evaluation, and management.
- Visentin GP & Liu CY (2007). Drug-induced thrombocytopenia.
- James N. George, MD; Gary E. Raskob, MSc; Shehla Rizvi Shah, MD; Mujahid A. Rizvi, MD; Stephen A. Hamilton, MD; Scott Osborne, BA; & Thomas Vondracek, PharmD (1998). Drug-Induced Thrombocytopenia.
8. Alcohol
Thrombocytopenia can also be common in serious alcoholics. This is a lifestyle-related cause of low platelets.
What causes platelets to be low when drinking alcohol? Although reduced platelet counts may be due to bone marrow suppression induced by alcohol, in this population group are two significant factors: lack of folate and hypersplenism because of chronic liver disease.
Thrombocytopenia in alcoholics can be generally mild to moderate, but we can find cases of severe thrombocytopenia, particularly when there are several factors involved (eg. Folate deficiency + bone marrow suppression induced by alcohol).
9. Heparin-induced thrombocytopenia
For every patient with a low platelet count, it is important to consider heparin-induced thrombocytopenia. It is because HIT patients are exposed to increased risk of thrombosis. Thrombocytopenia due to heparin can develop in 1% to 5% of patients. In most cases, this is what causes low blood platelets in just 6-10 days after the start of treatment with heparin.
However, if the patient has already received treatment with heparin in the past, thrombocytopenia may develop faster. It is important to understand that even low doses of heparin can cause thrombocytopenia. In fact, heparin-induced thrombocytopenia has been observed with the administration of heparin in low doses just for the purpose of flushing the vascular catheter.
It is believed however that low molecular weight heparin is less immunogenic and involved in only a few number of cases of thrombocytopenia compared to standard heparin. Remember, low platelets cause a risk of bleeding, especially if it will be a large drop.
Nonetheless, immune-mediated thrombocytopenia is still described in the use of low molecular weight heparin. Since the two types of heparin display a very pronounced cross-reactivity between them, it is often not possible, that even in the event of thrombocytopenia, to simply replace the use of standard heparin with that of low molecular weight.
In everyday clinical practice, withdrawal of thrombocytopenia following the lifting of heparin use confirms the diagnosis.

10. Hypersplenism
Hypersplenism is a fairly common cause of thrombocytopenia due to increased retention of platelets. In patients with hypersplenism, platelet count rarely falls to <30,000 / uL. A platelet count less than this should constrain the search for additional or other etiology.
Although, it may also be usually present in leukopenia and / or anemia, in some situations, it may only be displayed in cases of thrombocytopenia.
Detection of splenomegaly during physical examination is considered to support the diagnosis. However, studies have shown that physical examination does not always detect many cases of splenomegaly. Therefore, it may be necessary to perform estimations on the size of the spleen using imaging (eg. Ultrasound examination).

- Yunfu Lv, Wan Yee Lau, Yejuan Li, Jie Deng, Xiaoyu Han, Xiaoguang Gong, Ning Liu, & Hongfei Wu (2016). Hypersplenism: History and current status.
- Mohammad Hanafiah, Azura Mohamed Mukhari Shahizon, Soo Fin Low, & Man Harun Shahrina (2013). Severe thrombocytopenia due to hypersplenism treated with partial splenic embolisation.
- Júlio Cezar Uili Coelho; Priscilla Balbinot; Rodrigo Nitsche; Kátia Aparecida Pinto; Mônica Beatriz Parolin; & Cláudia Alexandra Pontes Ivantes (2011). Change in platelet count in patients with hypersplenism subjected to liver transplantation.
- READ MORE





Thank you for this essay on low platelet counts. I am a 71 year old male, type II diabetic who has been experiencing low platelet count for over 5 years. I am seeing a group that specializes in cancer treatment and blood disorders. Cancer is not thought to be the cause of my condition. I noted 3 medications in your essay that I’ve taken daily for up to 25 years. I have taken the following: Naproxen (1995-2000), Hydrocodone (2000-2010), Methadone (2010-2015), Fentynal (2015-2019), Ibuprofen (2019-November 2020), and Acetaminophen (starting 2 weeks ago). I take this under supervision of several physicians and Nurse Practitioners. They are from different practices, but all are completely aware of the meds I take. I experience severe pain almost every day. I injured my neck in a 90 mph motorcycle accident in 1970. I had 2 cracked vertebrae and a slipped disk, but had no continuous pain until an mva in 1995. Since 1995 I’ve experienced significant pain and headaches on a daily basis. I also experience pain in both knees, both hips, my right shoulder, and right wrist. One of the practitioners I see is a pain doctor. Most of these other painful areas result from many years of football. I also take Simvastatin once daily. I see these meds. are on your list of possible causes for my low platelet count. An additional medication I take is Eliquis. Since it acts as a blood thinner I wonder if that could be the culprit? I come from a long line of physicians and nurses. My wife is a Nurse Practitioner and my daughter is an Oncology Nurse. Myself, I have a degree in Finance and several strong minors: Computer Science, Engineering, Economics, and Mathematics. all of my physicians, nurse practitioner, my wife, and my daughter are collaborating to find the cause of my low platelets. This has been going on now for almost 6 years. During that time I’ve had dozens of blood checks and my platelet count has ranged from a high of just 55,000/uL – 15,000/uL. I just had another test last week and I’m back down to 15,000/uL I’m writing to see if you can suggest literature we might have missed. Again, thank you for what you;ve written. It’s comforting to read about potential causes in hope of finding a cure or treatment.
Sincerely,
Peter Agnew PDAgnew@gmail.com