High Platelet Count
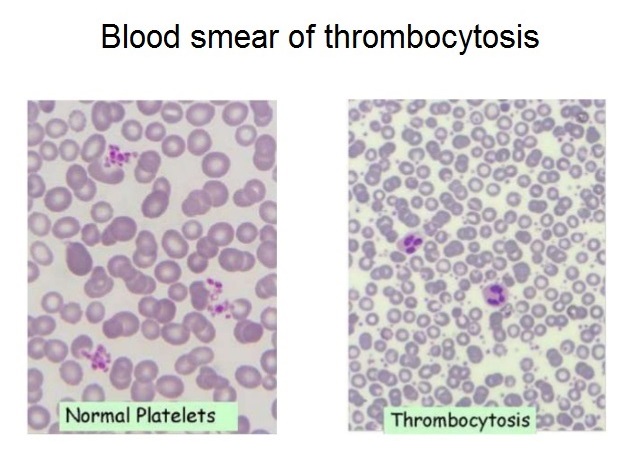
Platelets are small, oval/spherical component of the blood that don’t have its own nucleus. These small fragments are produced in the bone marrow and plays a very important part in blood clotting.
Normal levels of platelets in the blood is about 150-450×109 / L of blood. There are several factors that influence platelet life span but normally goes for only 7-10 days.
What causes high platelet count? Thrombocytosis is the medical term used to describe the display of elevated platelet count. The higher end of the normal platelet count range may vary from lab to lab, but is typically around 350 to 450 × 109 / L.
Doctors can detect thrombocytosis during routine blood tests. But there are specific blood platelet tests important for specific purposes. The display of increased level of platelets can be suggestive in determining reactive thrombocytosis or thrombocythemia, which is likely to cause abnormal blood clots. High platelet count in children can be different, you can read about it here.
With the information below, we will further identify what causes platelets to be high in some individuals. There are actually over 10 factors. Besides, you should also check out the most common platelet disorders.
The causes of high platelet count or thrombocytosis can be classified as follows:
- Physiological thrombocytosis
- Reactive (secondary) thrombocytosis
- Clonal (primary) thrombocytosis
I. Physiological thrombocytosis can be a result of:
- Exercise (workload)
- Stress
- Adrenaline
II. Reactive (secondary) thrombocytosis may result from:
- Acute blood loss
- Hemolytic anemia
- Infection
- Inflammatory diseases
- Iron deficiency anemia
- Malignant disease
- Surgery
- Post splenectomy / hypospleenism
- Drug reactions (vincristine, all trans retinoic acid, cytokines, growth factors)
- Feedback (“reactive”) thrombocytosis
- Trauma
Infection
A series of acute and chronic infection has been associated with reactive thrombocytosis. Megakaryopoiesis is inhibited in the presence of an acute infection which may be due to a virus or bacteria. This can help suggest and identify what causes a high platelet count in a patient who is experiencing either a viral or bacterial infection. Bacterial infections may be pneumonia, pyelonephritis, purulent arthritis, osteomyelitis, chronic wound infections, tuberculosis, among others. Viral infections, on the other hand, rarely reflects thrombocytosis.
Inflammatory diseases
Inflammatory diseases that can cause thrombocytosis are rheumatoid arthritis, rheumatic polymyalgia, polyarteritis nodosa, inflammatory bowel disease, nephritis and liver cirrhosis. Typically, the degree of severity of the disease condition corresponds to that of thrombocytosis. With proper treatment of the involved inflammatory disease/s, platelet count is very likely to return to normal levels.
Iron deficiency anemia
Elevated platelet count is not uncommon in patients with sideropenic anemia (group of anemias marked by low levels of iron in the plasma), specifically iron deficiency anemia. Sometimes platelet count may be greater than 1000 × 109 / L. Introducing iron replacement therapy helps the platelet count to generally return to normal within 10 days.
Malignant disease
There has also been a described association of thrombocytosis with many neoplasms, including Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, ovarian, bladder, mesothelioma, lung cancer, prostate and pancreatic cancer. About 90% of patients with reactive thrombocytosis due to a malignant disease displays a platelet count between 400 and 1000 × 109 / L.
Splenectomy
After splenectomy, a person may develop thrombocytosis that sometimes exceed 1000 × 109 / L. This removal of the spleen is what causes high platelets in some patients after the surgery. The platelet count usually returns to normal within a few weeks or months. Permanent thrombocytosis after splenectomy should give pause for thought about the existence of myeloproliferative disorder or any condition that may have developed like hemolysis or ineffective erythropoiesis.
Reactive thrombocytosis rarely causes symptoms.
But if symptoms occur, they may include the following:
- Headache
- Dizziness or lightheadedness
- Chest pain
- Weakness
- Unconsciousness
- Temporary changes in vision
- Numbness or tingling in the hands or feet
Treatment of Reactive Thrombocytosis
Treatment of reactive thrombocytosis is directed at the cause. If the cause is due to previous surgery or injury that have resulted to a significant loss of blood, thrombocytosis will not last long. If the cause is due to chronic infection or inflammatory disease, platelet levels may remain elevated until the condition is brought into control.
In most cases, the platelet count returns to normal after treatment of the root cause. But still, the removal of the spleen may cause a lifetime of thrombocytosis. In this case, the doctor may prescribe a low-dose aspirin to prevent bleeding as well as blood clotting, but which rarely occur in reactive thrombocytosis. Nevertheless, the patient should be cautious of blood clot symptoms.
III. Clonal or primary thrombocytosis may appear because of:
- Acute Megakaryocytic Leukemia (a rare subtype of AML)
- Myeloproliferative disease
- Essential thrombocytosis
- Polycythemia vera
- Agnogenic myeloid metaplasia
- Chronic myeloid leukemia
- Myelodysplastic syndrome
Chronic myeloid leukemia
Two-thirds of patients with chronic myeloid leukemia are found to have thrombocytosis.
Polycythemia vera
Increased platelet count has also been observed in approximately 66% of patients with polycythemia vera. About 5% of the patients have marked thrombocytosis (platelet count greater than 1000 x 109 / L).
Agnogenic myeloid metaplasia
Also known as idiopathic myelofibrosis, myeloid metaplasia agnogenic, is manifested by anemia and splenomegaly. A review of peripheral blood smear often detects Leukoerythroblastosis, described as a finding of erythrocytes in the form of tears, and immature precursors of red blood cells and leukocytes.
Thrombocytosis has been found in about 33% of patients with the condition, but in advanced stages of the disease, thrombocytopenia will usually be the significant finding.
For most myelodysplastic disorders, thrombocytosis is not typical. In fact, in most patients, it’s more often a display of normal or reduced platelet count. One form of myelodysplastic syndrome, called “5q-syndrome”, is associated with thrombocytosis in 50% of patients.
Essential thrombocytosis
Essential thrombocytosis, or primary thrombocythemia is a chronic disease characterized as a myeloproliferative neoplasm showing an enlargement in the total number of blood platelets.
The exact cause of essential thrombocythemia is not fully known, but it is assumed that there is a certain degree of genetic predisposition.
Some research shows that essential thrombocythemia is diagnosed in only about 6 persons per 100,000 people in one year. Males are equally affected as females, however in the younger population, a higher percentage favors women. This disease is more common among members of the older population, although one in five patients is younger than 40 years.
Source:
National Heart, Lung, and Blood Institute (Thrombocythemia and Thrombocytosis, Renal and Urology News (Thrombocytosis), Cancer Therapy Advisor (Thrombocytosis), Epocrates (Essential thrombocytosis)
Journal Reference:
- Radek C. Skoda, MD. Thrombocytosis. ASH Education Book, 01 Jan 2009; http://asheducationbook.hematologylibrary.org/content/2009/1/159.abstract
- Heng JT, Tan AM. Thrombocytosis in childhood. Singapore Medical Journal, 01 Nov 1998; http://europepmc.org/abstract/MED/10067383
- David H. Buss, M.D., Alan W. Cashell, M.D., Michael L. O’Connor, M.D., Frederick Richards II, M.D., L. Douglas Case, Ph.D. Occurence, etiology, and clinical significance of extreme thrombocytosis: A study of 280 cases. PlumX Metrics, 1994; https://www.amjmed.com/article/0002-9343(94)90150-3/abstract
- M. Mohamud, L. Osborne, H. G. Jones, A. Ahmed, J. Beynon, D. A. Harris, M. Evans, M. Davies, U. Khot, T. V. Chandrasekaran. Thrombocytosis as a Marker for Postoperative Complications in Colorectal Surgery. Gastroenterology Research and Practice, 2018; https://www.hindawi.com/journals/grp/2018/1978639/
- Andrew I. Schafer, M.D. Thrombocytosis. N Engl J Med, 2004 Mar; https://www.nejm.org/doi/full/10.1056/NEJMra035363
- Richard J. Lin, Vahid Afshar-Kharghan, Andrew I. Schafer. Paraneoplastic thrombocytosis: the secrets of tumor self-promotion. Blood Journal, 2014; http://www.bloodjournal.org/content/124/2/184
- READ MORE




My PLATELETS were high after COVIDinjection. And i had limes disease. Which was critical. It affected my speen. Dont know if these two things affected lab tests?